Originally posted May 28, 2025
What does male contraception look like in a post-Roe world? While the US government is increasing reproductive restrictions, interest in gender equity grows amidst surging online misinformation. It’s time to discuss men’s reproductive health responsibilities.
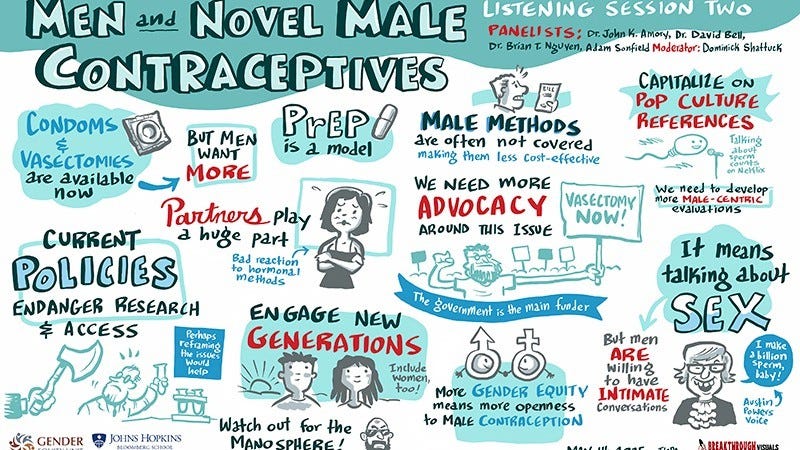
In a recent webinar hosted by Dominick Shattuck, PhD at Johns Hopkins and the Male Contraceptive Initiative, four experts: Dr. John Amory (University of Washington), Dr. David Bell (Columbia University), Dr. Brian T. Nguyen (University of Southern California), and policy analyst Adam Sonfield (Sonfield Policy Solutions LLC) took up these questions in an urgent and forward-looking conversation. Across their clinical, policy, and research perspectives, a consensus emerged: male contraception is not just a technological frontier; it’s a cultural one.
A Paradigm Shift: From Female Burden to Shared Responsibility
The discussion opened by acknowledging a long-standing imbalance: while women have historically borne the majority of contraceptive responsibility, there is growing evidence that men are both willing and eager to take on a more active role. A systematic review found that between 34% and 82% of men expressed willingness to use a novel male contraceptive method.1 Notably, women also indicated high levels of trust in their partners, with studies showing that 43% to as many as 94% would be willing to rely on a male partner to use contraception, underscoring the broad potential for shared responsibility in future contraceptive landscapes. 2-4
Yet, as Amory emphasized, creating a highly effective method means little if no one wants to use it. “If we develop a perfect male contraceptive, but nobody uses it, it’s a fairly limited victory,” he said, stressing the importance of human-centered design and user engagement. Nguyen echoed this sentiment, noting that while researchers have spent decades refining the science, they must now prioritize cultural context and end-user values, particularly around masculinity, trust, and relationship dynamics.
Masculinity, Altruism, and Reproductive Partnership
Bell offered a useful reframe by spotlighting the positive motivations he sees among his patients. Drawing on his work with adolescent and young adult men, he pointed to the role of altruism and care for partners’ well-being as underutilized levers. “Somewhere in there, there's altruism,” he explained. “Guys actually do care about their partner's health and want to mitigate side effects women may experience with female contraception.”
The language of partnership and care, rather than fear, control, or avoidance, has powerful implications. This framing challenges the often-cynical view that men are disengaged or unreliable in reproductive matters and invites a new narrative: one where men are active, empathetic, and morally invested participants.
Policy Gaps and the Manosphere
While there is reason for optimism, the panel also addressed substantial headwinds. Sonfield spoke to a hostile policy environment, particularly in schools, where basic sexual and reproductive health information is increasingly under threat. “We need to protect the right to information,” he urged, referencing efforts to conflate sex education with pornography and to remove any discussions about reproductive health from public school curricula.
He also highlighted the growing influence of the "manosphere"—a network of online spaces that promote hypermasculinity, misogyny, and reproductive disinformation. The threat, Sonfield warned, is not just cultural backlash but policy regression, such as renewed calls for spousal consent laws or male veto power over abortion. “We have to make sure male responsibility doesn't end up trampling women’s rights,” he said.
Intersectionality and Innovation
Nguyen’s insights bridged the clinic and the community. As a practicing OB-GYN and founder of the EMERGE Lab (Expanding Male Engagement in Reproductive and Gender Equity), he described how male reproductive health can be bundled with broader services, including HPV vaccination, STI testing, and even fertility counseling. This reduces stigma and increases system buy-in. “When you package contraception within broader male sexual health, it becomes more accessible and less controversial,” he explained.
He also emphasized that male interest in contraception correlates with gender equity. In countries where couples report higher rates of gender equity, men express more interest in contraceptive methods. These statistics provide a compelling reminder that structural context and individual behaviors are reinforcing factors in the health of our relationships and bodies.
Building the Infrastructure of Trust
If the science is advancing and the interest is there, what’s missing? Infrastructure, said Bell. He drew parallels between the rollout of PrEP (pre-exposure prophylaxis for HIV prevention) and the future of male contraception. PrEP programs have created clinical pathways, provider comfort, and demand generation mechanisms that male contraception could emulate. “We now have a model for male contraceptive care,” Bell said.
And, these systems require intentionality. Amory noted that male trials are still judged by female standards that include counting pregnancy as the endpoint, for example, rather than focusing on sperm suppression. “That (traditional) model doesn’t map well to men,” he joked, calling for new research frameworks and regulatory guidance.
Conclusion: Toward a Shared Future
The takeaway? Male contraception is not just a medical innovation; it’s a cultural and policy imperative. If developed with empathy, equity, and inclusion, it holds the promise of transforming not only reproductive health but gender norms themselves.
A final note from Sonfield captured the stakes well: “The more options we have that are universal… the more it becomes clear that contraception matters for everyone. And that might finally break the political cycle we’ve been stuck in for decades.”
We are, it seems, on the brink—not just of new products, but of new possibilities.
Reynolds-Wright, J. J., Cameron, N. J., & Anderson, R. A. (2021). Will men use novel male contraceptive methods and will women trust them? A systematic review. The Journal of Sex Research, 58(7), 838–849. https://doi.org/10.1080/00224499.2021.1905764
Roth, M. Y., Shih, G., Ilani, N., Wang, C., Page, S. T., Bremner, W. J., Swerdloff, R. S., Sitruk-Ware, R., Blithe, D. L., & Amory, J. K. (2014). Acceptability of a transdermal gel-based male hormonal contraceptive in a randomized controlled trial. Contraception, 90(4), 407–412. https://doi.org/10.1016/j.contraception.2014.05.013
Behre, H. M., Zitzmann, M., Anderson, R. A., Handelsman, D. J., Lestari, S. W., McLachlan, R. I., Meriggiola, M. C., Ng, E. M. L., Wittert, G., Wu, F. C. W., & Festin, M. P. R. (2016). Efficacy and safety of an injectable combination hormonal contraceptive for men. The Journal of Clinical Endocrinology & Metabolism, 101(12), 4779–4788. https://doi.org/10.1210/jc.2016-2141
Glasier, A. F., Anakwe, R., Guetta, R., Templeton, A., Levy, G., & Anderson, R. A. (2000). Would women trust their partners to use a male pill? Human Reproduction, 15(3), 646–649. https://doi.org/10.1093/humrep/15.3.646